
The development of vaccines against the Human Herpesvirus (HHV) family represents both one of the greatest successes and one of the most persistent challenges in modern vaccinology. The lifelong latency, sophisticated immune evasion mechanisms, and complex pathogenesis of these viruses demand innovative and multifaceted research and development strategies. Unlike acute viral infections, an effective HHV vaccine may need to do more than prevent initial infection; it might also need to control reactivation, reduce transmission, or even treat associated diseases.
At CD BioSciences, we are dedicated to advancing HHV research by supporting our partners in the pharmaceutical and biotechnology sectors. This article provides a comprehensive overview of the HHV vaccine R&D landscape, covering key vaccine types, cutting-edge technology platforms, and the current development status for major herpesviruses. This content is intended for research and informational purposes and does not constitute medical advice.
Vaccine Types: Prophylactic vs. Therapeutic Strategies
The goals of HHV vaccination can be broadly divided into two categories, each requiring a distinct scientific approach.
Prophylactic Vaccines
The primary goal of a prophylactic vaccine is to prevent initial infection or to significantly limit the severity of primary disease in uninfected (seronegative) individuals. The ideal prophylactic vaccine would induce robust, long-lasting sterilizing immunity, preventing the virus from ever establishing a latent reservoir. This requires the generation of potent neutralizing antibodies to block viral entry into host cells, as well as strong T-cell responses to clear any cells that do become infected. However, given the ability of HHVs to rapidly establish latency, even a partially effective prophylactic vaccine that reduces viral load and prevents clinical symptoms is considered a valuable public health tool.
Therapeutic Vaccines
A therapeutic vaccine is designed for individuals who are already latently infected (seropositive). Its purpose is not to prevent the initial infection but to enhance the host's immune control over the latent virus. The key objectives are to:
- Reduce the frequency and severity of reactivation episodes (e.g., recurrent genital herpes or shingles).
- Decrease asymptomatic viral shedding, thereby reducing transmission to others.
- Prevent or treat HHV-associated malignancies (e.g., EBV- or KSHV-associated cancers).
Therapeutic vaccines primarily aim to boost the cellular immune response, particularly cytotoxic T lymphocytes (CTLs), which are crucial for recognizing and eliminating virally infected cells during reactivation.
Vaccine Platforms & Technologies
The challenges posed by HHVs have driven the adoption and innovation of diverse vaccine platforms, moving far beyond traditional methods. The selection and validation of an optimal platform are critical preclinical decisions, often requiring specialized services in antigen expression, vector construction, and immunogenicity testing.
Live-Attenuated Vaccines
This traditional approach uses a weakened form of the virus that can replicate to a limited extent but does not cause disease. It elicits a broad immune response, including both antibody and T-cell immunity, closely mimicking natural infection. The first-generation varicella-zoster virus (VZV) vaccine (Varivax) and the shingles vaccine Zostavax are live-attenuated products. However, safety is a major concern, especially for immunocompromised individuals, as there is a risk of the attenuated virus reverting to a virulent form or causing disease itself.
Subunit Vaccines
Subunit vaccines are a much safer alternative, as they contain only specific, purified viral components (typically glycoproteins from the viral envelope) rather than the entire virus. These antigens are incapable of causing infection on their own. The major challenge is that these purified proteins are often less immunogenic than a whole virus. Therefore, they are almost always formulated with an adjuvant—a substance that enhances the body's immune response. The modern VZV vaccine, Shingrix, is a prime example of a highly successful subunit vaccine. It combines the VZV glycoprotein E (gE) antigen with the potent AS01B adjuvant system, generating a significantly stronger and more durable immune response than its live-attenuated predecessor.
mRNA Vaccines
Brought to the forefront by the COVID-19 pandemic, messenger RNA (mRNA) technology is a revolutionary platform for vaccine development. mRNA vaccines work by delivering a synthetic mRNA sequence that instructs the host's cells to temporarily produce a specific viral antigen. This in vivo production of the antigen elicits a powerful and broad immune response. Key advantages include:
- Speed and Flexibility: mRNA vaccines can be designed and manufactured rapidly.
- Potent Immunity: They can induce high levels of neutralizing antibodies and strong T-cell responses.
- Safety: They are non-infectious and do not integrate into the host genome.
This platform is now being aggressively pursued for complex viruses like Cytomegalovirus (CMV) and Epstein-Barr Virus (EBV), for which traditional approaches have been insufficient.
Viral Vector Vaccines
This platform uses a modified, harmless virus (the vector, such as an adenovirus or Modified Vaccinia Ankara virus) to deliver the genetic code for an HHV antigen into host cells. Like mRNA vaccines, this leads to the internal production of the target antigen, stimulating robust cellular and humoral immunity. This approach is being explored for therapeutic vaccines against HSV and other herpesviruses.
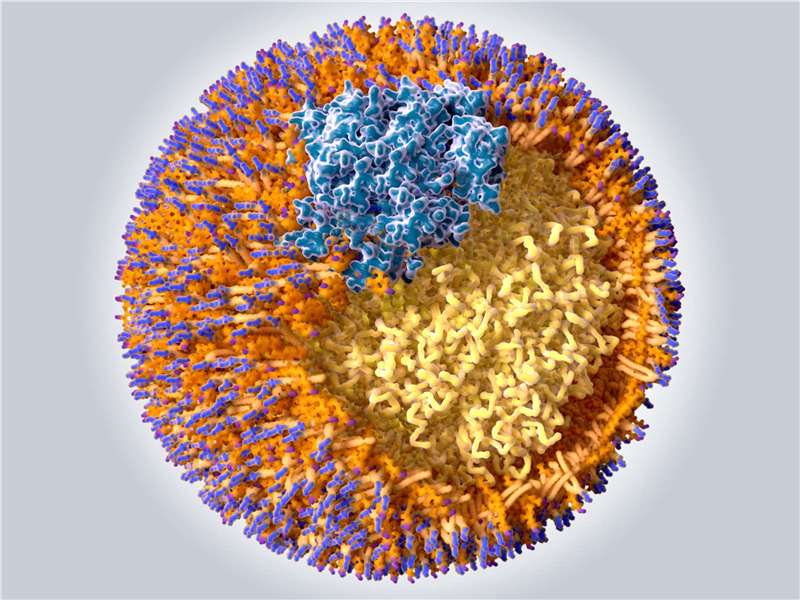
Virus-Like Particles (VLPs)
VLPs are multi-protein structures that mimic the overall structure of a native virus but contain no viral genetic material, making them non-infectious. Because they closely resemble the authentic virion structure, they are highly effective at stimulating the immune system, particularly B-cell responses, to produce high-titer neutralizing antibodies. VLP-based strategies are a promising avenue for several HHV vaccine candidates.
Development Landscape
The progress in vaccine development varies significantly across the HHV family, reflecting the unique biology and clinical impact of each virus.
- Varicella-Zoster Virus (VZV)
VZV is the standout success story. The live-attenuated Varivax prevents chickenpox in children, and the recombinant subunit vaccine Shingrix is over 90% effective at preventing shingles in older adults. The success of Shingrix, in particular, has provided a powerful blueprint for other HHV vaccines, demonstrating that a well-chosen subunit antigen combined with a powerful modern adjuvant can overcome age-related immune decline and effectively control reactivation.
- Herpes Simplex Virus 1 & 2 (HSV-1, HSV-2)
Developing a vaccine for HSV has been a goal for decades, marked by numerous clinical trial failures. The complexity of the virus, its potent immune evasion mechanisms, and the difficulty in identifying the right combination of antigens have made this a formidable challenge. Past efforts focusing on envelope glycoproteins gD and gB have not yielded sufficient efficacy. The field is now shifting towards:
Therapeutic Vaccines
Many current efforts focus on controlling recurrent disease in the millions already infected.
Novel Platforms
mRNA and viral vector approaches are being tested to elicit a more potent and targeted T-cell response.
New Antigens
Researchers are exploring different antigens beyond the standard glycoproteins, including those expressed during latency, to create a more effective therapeutic response.
- Cytomegalovirus (CMV)
A prophylactic CMV vaccine is a major public health priority due to its role as the leading infectious cause of congenital birth defects. The virus has a large, complex genome with multiple mechanisms to evade the immune system. After years of limited progress, the field is now energized by Moderna's mRNA-1647, a vaccine candidate currently in a pivotal Phase 3 clinical trial. This vaccine contains mRNA encoding for six different viral proteins (five for the pentamer complex, which is crucial for entry into endothelial and epithelial cells, and one for glycoprotein B), representing a sophisticated, multi-pronged attack on the virus.
- Epstein-Barr Virus (EBV)
EBV is associated with infectious mononucleosis and several types of cancer, including nasopharyngeal carcinoma and lymphomas. It is also increasingly implicated in autoimmune diseases like multiple sclerosis. For years, EBV vaccine development was a low priority for major manufacturers. However, spurred by the success of mRNA technology and the growing recognition of EBV's role in disease, multiple candidates are now in development. Both the U.S. National Institutes of Health (NIH) and Moderna have initiated early-stage clinical trials for prophylactic EBV mRNA vaccines targeting multiple viral glycoproteins.
- Kaposi's Sarcoma-associated Herpesvirus (KSHV/HHV-8)
Vaccine development for KSHV is the least advanced among the major HHVs. Research is largely in the preclinical phase, focused on identifying protective antigens and establishing a viable vaccine platform. The primary target population would be individuals in regions with high KSHV prevalence (like sub-Saharan Africa) and immunocompromised patients, such as those with HIV or organ transplant recipients, who are at high risk for Kaposi's sarcoma. Advancing a KSHV vaccine will rely on foundational research supported by specialized products and services.
Conclusion
The HHV vaccine R&D landscape is a dynamic and challenging field, but one that is experiencing a renaissance driven by next-generation platforms like mRNA and advanced adjuvanted subunit technologies. While VZV provides a model for success, viruses like HSV, CMV, and EBV continue to present significant hurdles that demand persistent and innovative preclinical research. Success will depend on a deeper understanding of viral immunology, the identification of optimal antigens, and the robust preclinical evaluation of new vaccine candidates.
References
- Whitley, R. J., & Baines, J. (2018). The Varicella-Zoster Virus Vaccine: A Decade of Experience. The Journal of Infectious Diseases, 218(suppl_2), S56–S62. https://doi.org/10.1093/infdis/jiy421
- Lal, H., Cunningham, A. L., Godeaux, O., et al. (2015). Efficacy of an adjuvanted herpes zoster subunit vaccine in older adults. New England Journal of Medicine, 372(22), 2087-2096. https://doi.org/10.1056/NEJMoa1501184
- Johnston, C., & Koelle, D. M. (2022). Herpes simplex virus vaccine development: A renewed sense of urgency. The Journal of Infectious Diseases, 226(Supplement_1), S1-S3. https://doi.org/10.1093/infdis/jiac238
- Rieder, F., & Steininger, C. (2014). Cytomegalovirus vaccine: a long and winding road. Expert Review of Vaccines, 13(3), 377-387. https://doi.org/10.1586/14760584.2014.882481
- Cohen, J. I. (2023). Epstein-Barr virus vaccines. Clinical and Translational Immunology, 12(3), e1453. https://doi.org/10.1002/cti2.1453
- ModernaTX, Inc. (2024). A Study to Evaluate the Efficacy, Safety, and Immunogenicity of mRNA-1647, a Cytomegalovirus (CMV) Vaccine, in Healthy Participants 16 to 40 Years of Age (CMVictory). ClinicalTrials.gov Identifier: NCT05085366. https://clinicaltrials.gov/study/NCT05085366