
The global prevalence of human herpesviruses (HHVs) presents a persistent challenge to public health. While these viruses establish lifelong latency, they cause a wide spectrum of diseases, ranging from mild mucocutaneous lesions to severe, life-threatening conditions, particularly in immunocompromised individuals. For decades, antiviral chemotherapy has been the cornerstone of managing active HHV infections. However, the emergence of drug-resistant strains, dose-limiting toxicities, and the inability of current drugs to eradicate latent viral reservoirs underscore the urgent need for a new generation of antiviral therapies.
This article provides a comprehensive overview of the dynamic field of HHV antiviral drug research and development. We will explore the key molecular targets being pursued, the diverse therapeutic strategies under investigation, and the current R&D landscape. This knowledge is critical for biotechnology companies, pharmaceutical developers, and academic researchers dedicated to creating safer and more effective treatments for HHV-associated diseases.
At CD BioSciences, we are committed to advancing HHV research by providing specialized products, services, and solutions that support every stage of the pre-clinical drug discovery pipeline.
Key Drug Targets in HHV Antiviral Development
The success of any antiviral drug hinges on its ability to selectively inhibit a viral process without causing significant harm to the host. The search for ideal drug targets is focused on proteins and pathways that are essential for the viral lifecycle and distinct from their host cell counterparts.
- Established and Emerging Viral Enzyme Targets
Viral enzymes remain the most validated and fruitful class of antiviral targets due to their critical roles in replication.
DNA Polymerase
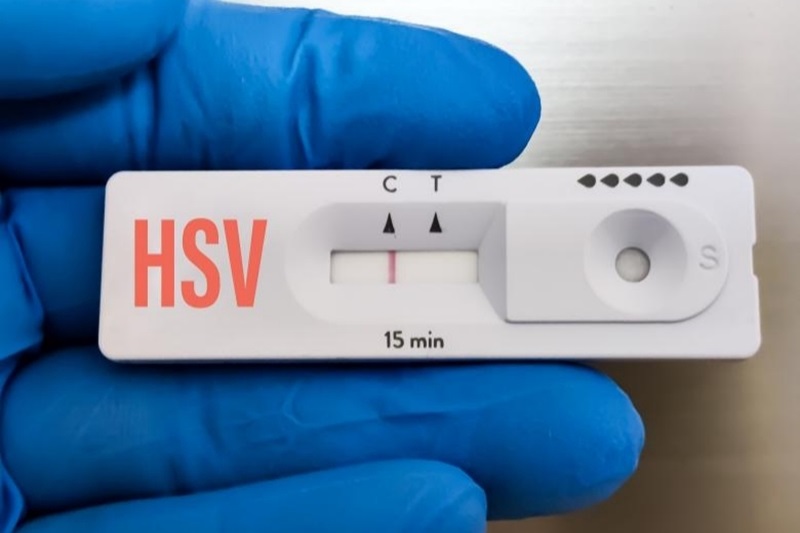
This is the most successful HHV drug target to date. The vast majority of approved anti-herpesvirus drugs, including nucleoside analogs like acyclovir (for HSV/VZV) and ganciclovir (for CMV), function by targeting the viral DNA polymerase. These drugs act as chain terminators after being phosphorylated by viral and/or cellular kinases, thus halting viral DNA synthesis. Non-nucleoside inhibitors like foscarnet bind to a different site on the polymerase and also block its function. However, mutations in the genes encoding the DNA polymerase or the activating viral kinases (e.g., UL97 in CMV, TK in HSV) can lead to significant drug resistance, driving the search for alternatives.
Helicase-Primase Complex
This three-protein complex (composed of UL5, UL8, and UL52 in HSV) is responsible for unwinding the double-stranded viral DNA at the replication fork and synthesizing RNA primers. Its essential, virus-specific function makes it a highly attractive target. The development of helicase-primase inhibitors, such as pritelivir, represents a major advancement. These drugs act via a novel mechanism, directly inhibiting enzymatic activity and offering an effective treatment option for acyclovir-resistant infections.
Terminase Complex
Following DNA replication, the viral terminase complex is responsible for recognizing, processing, and packaging newly synthesized viral genomes into pre-formed capsids. This process is unique to the virus and has no cellular equivalent, ensuring high specificity. Letermovir, approved for CMV prophylaxis in hematopoietic stem cell transplant recipients, validates this complex as a drug target. It inhibits the terminase complex (pUL51, pUL56, pUL89) and prevents the formation of infectious virions.
Viral Protein Kinases
HHVs encode their own protein kinases that regulate numerous viral and cellular processes, including the crucial first phosphorylation step of many nucleoside analog drugs. For example, CMV's UL97 protein kinase phosphorylates ganciclovir. Maribavir is a new-class drug that specifically inhibits the UL97 kinase, preventing viral DNA replication, encapsidation, and nuclear egress. It is effective against ganciclovir-resistant strains that carry UL97 mutations.
- Novel Targets for Future Therapies
Beyond classical enzymes, researchers are exploring other viral and host proteins.
Host Factors: Instead of targeting the virus directly, host-directed antivirals (HDAs) aim to inhibit cellular proteins or pathways that the virus hijacks for its own replication. This approach could have a higher barrier to resistance and potentially broad-spectrum activity. Targets include host cyclins, kinases, and metabolic pathways essential for viral propagation.
Latency-Associated Targets: The ultimate goal in HHV therapy is to target the latent reservoir. This is exceptionally challenging, as latent viruses exhibit minimal gene expression. Research is focused on understanding the molecular mechanisms that maintain latency, with potential targets including latency-associated transcripts (LATs) in HSV-1 or viral proteins essential for episome maintenance, such as EBNA1 in EBV and LANA in KSHV. Strategies aim to either permanently silence the latent genome or to induce a controlled reactivation followed by elimination with a conventional antiviral (a "shock and kill" approach).
CD BioSciences supports the critical early stages of discovery by providing a suite of tools, including high-purity recombinant viral proteins and tailored enzymatic assay development services, to help researchers validate and characterize these key drug targets.
Therapeutic Strategies in the R&D Pipeline
With a growing list of validated targets, researchers are employing a diverse range of strategies to develop next-generation HHV therapeutics.
- Direct-Acting Antivirals (DAAs)
This remains the primary strategy, involving the design of small molecules that directly bind to and inhibit a specific viral protein. The development of inhibitors against the helicase-primase and terminase complexes are prime examples of this strategy's ongoing success. The focus is on improving specificity, reducing off-target toxicity, and creating compounds active against resistant viral strains.
- Host-Directed Antivirals (HDAs)
This strategy is gaining traction as our understanding of virus-host interactions deepens. By targeting cellular factors, HDAs can circumvent viral resistance mechanisms. However, the development of HDAs requires a careful balancing act to ensure potent antiviral activity without causing unacceptable host toxicity, as these pathways may be important for normal cell function.
- Immunomodulatory Therapies
Given that the immune system is the primary force controlling HHV latency, strategies to boost or restore host immunity are highly promising.

Therapeutic Vaccines
Unlike prophylactic vaccines, these are designed to stimulate an immune response in already-infected individuals to better control viral reactivation.
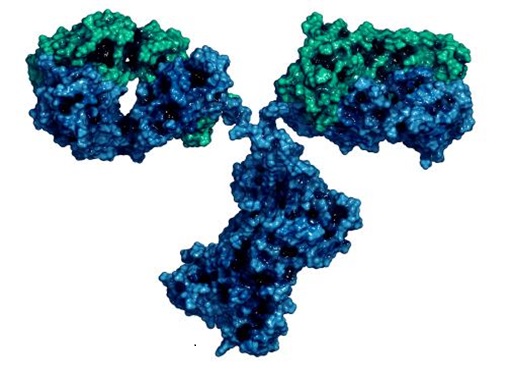
Monoclonal Antibodies (mAbs)
mAbs can be engineered to target viral glycoproteins, neutralizing free virions, or to block viral entry. They can also be used to target infected cells for destruction by the immune system.
Adoptive T-Cell Therapy
This involves isolating and expanding virus-specific T-cells from a donor or patient and infusing them back into the patient. This has shown significant success in post-transplant settings for controlling CMV and EBV infections.
- Combination Therapies
Drawing lessons from the success of HIV combination antiretroviral therapy (cART), researchers are exploring combination regimens for HHV. Using two or more drugs with different mechanisms of action can produce a synergistic effect, increase potency, and significantly lower the probability of developing drug resistance. For example, combining a DNA polymerase inhibitor with a terminase inhibitor could attack two distinct stages of the viral lifecycle.
Our team supports the pre-clinical evaluation of these diverse therapeutic strategies, offering services from high-throughput in vitro antiviral screening to the development of custom cell-based assays that model specific aspects of the HHV lifecycle.
The R&D Landscape: Challenges and Future Directions
The HHV antiviral R&D landscape is more vibrant and promising than ever before, but significant challenges remain.
- Overarching Challenges
Viral Latency
The inability to clear the latent viral reservoir is the single greatest challenge. A true cure for any HHV will require a solution to this problem.
Drug Resistance
The continuous evolution of viruses under drug pressure necessitates a robust pipeline of new drugs with novel mechanisms of action.
Predictive Pre-clinical Models
Developing accurate in vitro and in vivo models that can faithfully replicate the complexities of HHV infection, latency, and reactivation is crucial for translating basic research into clinical success.
Target Patient Populations
Many severe HHV diseases occur in specific, often vulnerable, populations like transplant recipients, cancer patients, or neonates, which can present unique challenges for clinical trial design and execution.
- Emerging Trends and the Path Forward
The future of HHV drug development will be shaped by technology and innovative thinking. High-throughput screening (HTS) and high-content imaging are accelerating the identification of new lead compounds. The application of artificial intelligence (AI) and machine learning is beginning to revolutionize drug design and target prediction.
The recent approvals of letermovir and maribavir for CMV have revitalized the field, demonstrating that novel targets can lead to clinically meaningful breakthroughs. The pipeline for HSV continues to focus on overcoming acyclovir resistance and exploring topical formulations, while research into EBV and KSHV-associated cancers is heavily invested in immunotherapies and targeted agents.
Navigating this complex landscape requires a partner with deep expertise in virology and drug development. CD BioSciences provides a comprehensive portfolio of HHV-focused pre-clinical solutions—from target validation and compound screening to mechanism of action studies—designed to help our clients de-risk their programs and accelerate the journey from discovery to the clinic.
References
- De Clercq, E., & Li, G. (2016). Approved Antiviral Drugs over the Past 50 Years. Clinical Microbiology Reviews, 29(3), 695–747. https://doi.org/10.1128/CMR.00102-15
- Poole, C. L., & James, S. H. (2018). The Holy Grail: Targeting Herpes Simplex Virus Latency. Viruses, 10(10), 561. https://doi.org/10.3390/v10100561
- Hwang, S., & Gentry, B. G. (2019). The Holy Trinity of Herpesvirus Replication: Helicase, Primase, and Polymerase. Viruses, 11(2), 136. https://doi.org/10.3390/v11020136
- Chou, S. (2021). Maribavir: A Novel Benzimidazole Riboside for Treatment of Cytomegalovirus Disease. Current Opinion in Investigational Drugs, 22(8), 1-13. (Note: Reference style may vary, providing a representative example).
- Hamarsheh, O. (2020). Host-directed therapy for the management of viral infections. Signal Transduction and Targeted Therapy, 5(1), 185. https://doi.org/10.1038/s41392-020-00299-8